The MHC has added new beds and services, effectively increasing access to treatment
In 2016, the MHC ran an efficient tender process that opened the market to appropriate new providers and expanded the options available. This added 52 residential rehab beds, 8 withdrawal beds and 13 CADS staff[2] to the existing network of drug and alcohol services. A specialist meth clinic was also set up to run high a medical withdrawal service, and funding was provided for frontline drug support nurses in hospital emergency departments. A dedicated meth helpline was also established.
The clinic differed from other AOD outpatient services. It involved intensive patient/client follow up, the trialling of pharmacotherapy to reduce withdrawals, and the offer of a 5 step cognitive behavioural therapy program.
Since the end of the funding, the clinic clients are treated as part of the mainstream outpatient service. The helpline is still active but frontline drug support nurses are no longer employed.[3] All other services are funded through to 2021.
These additions were based on a reasonable assessment of need, and have led to increased use. Between 2012-13 and 2016-17, the number of treatment episodes for all drugs increased 30% from 14,787 to 19,233.
The MHC’s tender process was comprehensive and completed as quickly as could be expected. It asked for expressions of interest on 11 July 2016 for 24 metropolitan and 28 regional residential rehab beds and 4 metropolitan and 4 regional withdrawal beds. It received applications from 10 providers, covering the South West, Midwest, Goldfields, Pilbara and all metropolitan regions. After clear and well-structured assessments and approvals, the process granted new or extended contracts to 6 providers in October 2016 (Table 1).
In January 2018, there were 439 residential rehab beds and 44 withdrawal beds, an increase of 20% and 24% respectively since October 2015. Of these MHC was funding 249 of the residential rehab beds and 42 of the withdrawal beds.
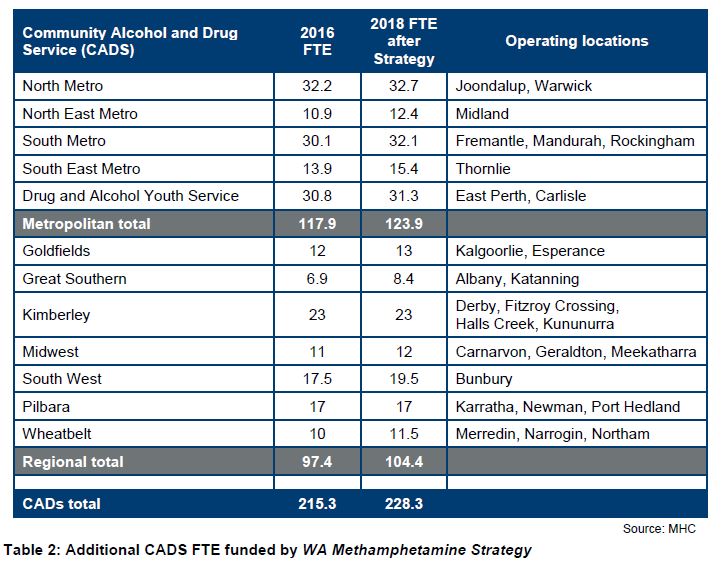
Under the WA Methamphetamine Strategy, $3 million was allocated to add the equivalent of 13 full-time staff (FTE) to CADS services (Table 2). An additional $4.5 million was allocated to continue this staffing level from 2018-19 to 2020-21. The positions are for counselling, information and referral for people who need help with meth and their families. These choices were based on a strong assessment of:
- the prevalence and severity of the problems being experienced with meth in each CADS catchment
- the existing community treatment and prevention workforce capacity at each CADS catchment
- the estimated population increases for WA
- high priority areas in Better Choices. Better Lives.
Despite the increases in treatment services, there is evidence that capacity does not yet meet demand
While these additional beds and CADS have increased the amount of service provided, the number of beds does not yet match that forecast in Better Choices. Better Lives, and waiting times indicate unmet need for CADS services. Measuring unmet demand is difficult. People who need treatment do not always admit to having a problem in the early period of their dependency. A range of personal, social and legal issues cause people to avoid treatment and also drop out of treatment, while privacy concerns make data collection challenging.
Despite this uncertainty, Better Choices. Better Lives estimated future need for services using national modelling tools applied to the population of WA.[4] This identified an optimal mix and level of mental health, alcohol and other drug services but did not separately identify the specific needs of people dealing with meth dependency.
Despite exceeding the estimated residential rehabilitation bed requirements for 2017 in total, MHC estimates show a shortfall in the north metropolitan area of 101 residential rehab beds (Table 3). MHC modelling also shows there are 18 fewer withdrawal beds across the state than were needed by 2017. It is not clear if these shortfalls accurately reflect current shortfalls in treatment capacity. However, providers report that demand is growing and they have to put people on waitlists for treatment.
The MHC has recognised the need to increase service capacity. It is currently seeking expressions of interest to create 30 new residential rehab beds and 3 low medical withdrawal beds in the South West following a commitment by the Government in the 2017 Methamphetamine Action Plan to target regional areas.
A similar situation applies to demand for CADS services. Even after the increase of 13 FTE for CADS counselling services, the total FTE of 228.3 is less than 20% of the 1,178.5 MHC’s modelling estimated would be needed by the end of 2025. It is unlikely this will be reached but a more up to date estimate of need could provide a more accurate estimate of any capacity shortfall.
People are using the extra services and average wait times have improved substantially, but some people are still not getting help when they need it
There has been a significant increase in the amount and proportion of AOD treatment undertaken by people with meth issues. Annual total treatments where meth was the main drug of concern increased by 38% from 5,482 in 2014-15 to 7,573 in 2016‑17, covering the period when the Strategy was introduced. Residential rehab treatments for people with a major meth problem grew by 74% in the same period and have more than doubled since 2012-13. (Figure 1). The increases in treatment episodes since 2014-15 indicate that the extra services are meeting the intent of expanding the services.
Meth has replaced alcohol as the major source of demand for treatment, increasing demand for residential rehab services:
- In 2012-13 alcohol was the major cause of treatment, with 44% of all cases. By 2016‑17 it was meth, making up 39% of cases.
- Treatment episodes where meth was the main drug of concern increased by 121%, from 3,421 to 7,573.
- In 2012-13, 162 people with a major meth problem received residential rehab treatment. In 2016-17 the number was 582, an increase of 259%.
While treatment numbers are increasing, there are still shortfalls across all service types. In the 3 months to January 2018, 5% of those on waitlists waited longer for metro CADS support than priority standards require. Another 9% left the system without getting treatment. This suggests that 1 in every 7 people seeking treatment are either not being seen in time or are dropping off the waitlist. It is not clear if this is acceptable to the MHC or should be improved. There was no information on non-metropolitan CADS. Average wait times for CADS appointments have improved substantially. Median times have also dropped, showing more people are being seen more quickly (Table 4).
At January 2018, 33 residential rehab beds were unoccupied, all but 2 of them in Geraldton. The vacancies in Geraldton were due to a change in service delivery which required all clients to do farm work. The provider has also introduced a strict no smoking policy which appears to have discouraged some people from using that service. The MHC is monitoring this situation.
A decrease in the Meth Helpline budget potentially reduces accessibility to counselling services. There were 1,447 calls to the Meth Helpline in the 12 months to 18 May 2018. In July 2018, the MHC confirmed the helpline’s budget had dropped by $154,000 for 2018-19, due to the end of funding from the Strategy. The Meth Helpline is staffed by the Alcohol and Drug Support Service (ADSS) and, though the Meth Helpline is still active, there are now 10 fewer ADSS shifts per fortnight, decreasing from 75 to 65.
[2] Full-time equivalent. The number of individuals doing the work will be greater if some are part-time.
[3] St John of God Hospital in Bunbury has continued with this initiative at its own expense.
[4] Better Choices. Better Lives p104.