Ambulance ramping has increased
Ambulance ramping has been increasing in recent years despite attempts by the DoH and SJA to reduce it. To date, ramping has not typically affected emergency cases because these are given highest priority but it has reduced average response times for lower priority cases, as ramping affects the number of ambulances available to respond to other calls. SJA fell short of response time targets for lower priority cases more often, and by a greater margin in 2017-18 whenever total ramped time of all ambulances at metropolitan hospitals added up to more than 24 hours in a day.
Ambulance ramping is the practice of leaving ambulances parked outside hospitals while crew wait with patients for admission to ED. Patients do not wait in ambulances but are taken on stretchers into the hospital where they are looked after by the ambulance crew until they can be handed over to the care of a nurse or doctor.
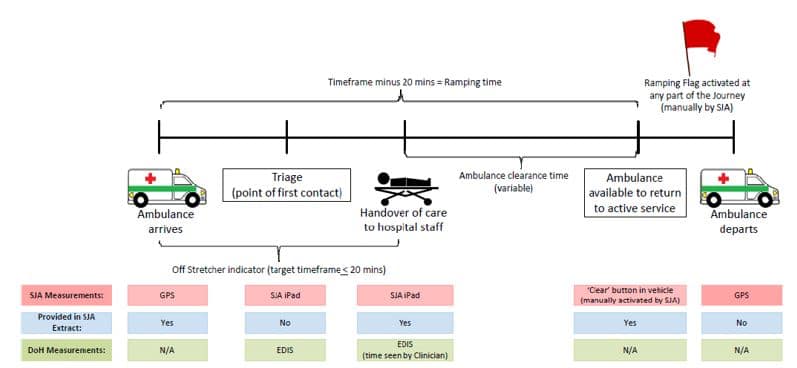
In SJA’s contract, ramping time is measured as the time elapsed from 20 minutes after the ambulance arrives at the ED to when the ambulance is cleared to respond to another call. Hospitals also record the time when they take over care of the patient. This is referred to as the ‘off stretcher’ time. Ramping time focuses on the ambulance while the off-stretcher time focuses on the patient. Both are recorded and reported to the DoH.
For both measures, the ambulance’s arrival is automatically recorded, while off-stretcher and clear times are manually recorded by the hospital or ambulance crew (Figure 6). Time to clear is almost always longer than the off-stretcher time because it includes time to clean-up and re-stock the ambulance. If the patient is left in the care of another ambulance crew then the off-stretcher time might exceed ramping time.
Source: Department of Health
Figure 6: Ambulance ramping sequence and measurement from arrival to departure. Note: EDIS stands for Emergency Department Information System.
Whatever measure is used, data shows that ramping has increased in recent years (Figure 7). It is highly visible and the subject of public and parliamentary concern.
Source: OAG from SJA data supplied to the DoH
Figure 7: Ambulance ramping (time to clear) for all ambulances at metropolitan hospitals by hours: January 2013 to March 2019 Note: broken red line is the trend line
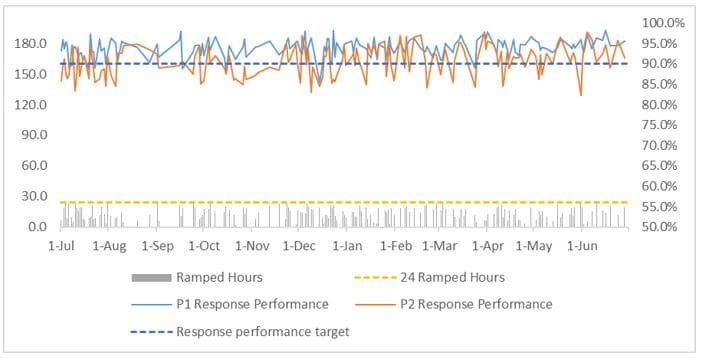
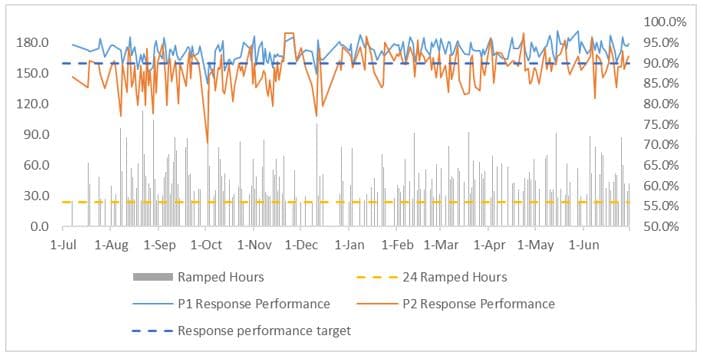
While response time in Priority 1 (emergency) cases was largely unaffected by ramping in 2017-18, SJA data shows response time targets for Priority 2 cases were met less often when total daily ramping time for all ambulances exceeded 24 hours (across all metropolitan hospitals on a particular day). Figure 8 shows the effect on response times when daily total ramping time was less than 24 hours. Figure 9 shows the effect on response times when total ramping times exceeded 24 hours. Overall, Priority 2 response performance was 90.5% for days when total ramping time was less than 24 hours and 88.4% when they exceeded 24 hours.
Source: OAG from SJA data
Figure 8: Daily priority 1 and 2 response times when total daily metropolitan ambulance ramping hours were under 24 hours: 2017-18
Source: OAG from SJA data
Figure 9: Daily priority 1 and 2 response times when total daily metropolitan ambulance ramping hours were over 24 hours: 2017-18
Figure 8 shows days where total ramping time was below 24 hours. Figure 9 shows days where total ramping time exceeded 24 hours. Ramped hours (left axis) is the total ramping time of all ambulances on a particular day. Response performance (right axis) is the percentage of times response times met their targets. Priority 1 response performance is generally above the 90% target in both scenarios, while Priority 2 drops below target when ramping exceeds 24 hours.
There is little evidence of ramping’s impact on patients’ health outcomes or system costs
Despite the increase in ramping of lower priority patients and the potential for discomfort this may cause, there is little available evidence that these patients suffer long term health impacts as a result. We also found little evidence that ramping imposes material costs on the health system.
While lower priority patients spend more time on ambulance stretchers during times of significant ramping, it may not be affecting their health outcomes. This may be because patients remain on ambulance stretchers and are cared for by ambulance crew during this time. This means they are more closely monitored than patients who present themselves to the ED and take their place unattended in the waiting room.
While it seems intuitively obvious that delays in treatment increase the likelihood of adverse outcomes, much depends on the nature of the condition that brought the patient to hospital. Conditions that require hospital treatment may not pose any immediate threat to the patient’s general health, and urgent pain management is often delivered effectively by ambulance crews. If a patient’s condition deteriorates while being attended by ambulance crew, the priority level can be increased and the patient taken into the ED without further delay.
We also found little evidence that ramping imposes material costs on the health system. While some hospitals have incurred costs in managing the queue of patients waiting with ambulance crew, these costs appear minor in the context of the system as a whole. Some hospitals have hired ambulance officers to help manage patient flow from ambulance deliveries. Other hospitals have hired nurses for this purpose. However, these costs should be seen in the context of the total cost of patient care, wherever it is needed. It is not clear that transferring these costs between the ambulance service and the hospitals would significantly reduce costs overall.
The DoH and SJA do not have an agreed plan or strategy to reduce ramping
The DoH and SJA meet at senior levels to address complex issues but have not found a way to reduce ramping. This may be because ramping affects hospitals and the ambulance service differently in patient, performance, and cost terms, making an effective joint approach hard to achieve.
Rather than focus on ramping as an isolated issue, it may be better to address it as a problem of managing patient flow into and through the hospital system. Hospitals we spoke to told us that delays in transport for mental health patients often led to them occupying ED beds for long periods, contributing to congestion in EDs and ramping. The DoH has established 2 mental health observation areas in EDs to manage mental health patients and reduce congestion, and advise that further measures are planned.
SJA has tried to reduce ramping by diverting patients away from hospitals when their need for treatment can be met by other means. SJA has established urgent care centres as an alternative for low acuity patients who might otherwise present themselves to an ED. These measures have not made a significant difference to ramping levels.
One reason urgent care centres have not significantly impacted ramping may be that these centres do not treat the large and growing number of ambulance patients who are over 65 years old. It is also possible that most ambulance patients require hospital treatment. Other proposed solutions to ramping include a central command centre with an overview of both ambulances and EDs, along with secondary clinical triage options. There is evidence from overseas that this could help but it would require substantial investment and a joint commitment by the DoH, Health Service Providers and SJA.
The causes of ramping are unclear but it seems to be a symptom, like a traffic jam, of a broader problem of managing patient flow into and through the hospital system. On this view, ramping occurs because of bottlenecks in the system and cannot be reduced by focusing on ambulances alone. Staff in the DoH, WACHS and SJA suggested that a centralised command centre with an overview of both ambulances and EDs could be a way forward.
Understanding the trigger point at which ramping will further affect ambulance response times and patient outcomes is important to help inform future capacity investment decisions, such as whether or when more ambulances and crews are required. This has not yet been done by the DoH and SJA.
One important contributing factor appears to be that mental health patients occupy ED beds for long periods while waiting for more appropriate accommodation. This creates congestion in EDs and contributes to low acuity ambulance patients being queued. Addressing this issue has the potential to improve patient flow and ease congestion in EDs, which in turn could ease ramping.
A factor limiting hospitals’ ability to move mental health patients out of EDs is a provision of the Mental Health Regulations 2015 that has been interpreted to limit mental health patient transport to contractors, thereby excluding hospital employees. This means that hospital staff cannot transport mental health patients and must rely on SJA which is contracted to run only 1 dedicated mental health transport crew.
A consequence is that mental health transport is not always available when needed. Providing for better mental health transport options in the SJA contract could improve this situation. Other factors, such as the availability of police or other qualified people to travel with high risk patients, could also be contributing to the problem.
During our audit, the DoH began a 3-month trial of expanded mental health transport. On 1 April 2019, SJA and another provider were engaged to provide 3 mental health crewed ambulances for 18 hours per day from 6 am to midnight. The DoH told us there were positive early results of the trial so it has extended the trial to June 2020 in the lead up to the new ambulance service contract.
The DoH addresses complex issues with SJA at CEO level through the WA Ambulance Standing Committee. This committee meets quarterly or as necessary to consider SJA reports and issues needing attention (e.g. ramping) as well as planning (e.g. the Winter Strategies). Contract management meetings are held more frequently. To date neither the Standing Committee nor the contract management process have found a way to permanently reduce ramping.